Chronic non-cancer pain – Making better decisions using opiates
May 12, 2020
Jeanine Bradley, RPh, Cert. MTM, Ch Herbalist
Let’s start with a little history… Opium is the air-dried milky substance created by the unripe capsule of Papver somniferum. Breaking it down one step more, the term opium comes from the Greek word Opion, meaning poppy juice. Papver is the Latin name of poppy and somniferumis in Latin means to produce sleep. The earliest use of Opium dates back to 3400 B.C. – it was known as the joy plant. Opium was known to the Greeks and Roman physicians as a powerful pain reliever. It was also used to induce sleep and to give relief to the bowels. In 1806, a German pharmacist became the first person to extract morphine from opium. That’s how it all got started.
To recap, opiates are naturally occurring chemicals found in the opium plant. The most well known opiates found include Morphine, Codeine, and Thebaine. They’re three of the oldest pain medications and doctors still prescribe them today. However, Thebaine isn’t used as a pain medication in its natural state. It is converted into other chemicals, such as oxycodone or hydrocodone, which are used in the popular medications Percocet and Vicodin, respectively. Oxycodone, Hydrocodone and Hydromorphone are examples of semi-synthetic opioids. Semi- synthetic opioids are man-made chemicals that are derived from naturally occurring opiates. Diacetylmorphine, more commonly known as heroin, is another example of a semi-synthetic opiate. Heroin is manufactured by boiling morphine and acetic anhydride.
Scientists have also created drugs in laboratories that mimic the effects of opiates but are not derived from the opium poppy. These drugs are known as synthetic opioids; examples include Methadone (Methadose), Fentanyl (Duragesic), Meperidine (Demerol) and Tramadol (Ultram).
The 1970 Controlled Substance Act categorized medications into a 4 Schedule classification of those agents that can cause psychological dependence, physical dependence, manifest a medical value and/or potential for abuse or addiction. The Controlled Substance Act serves as the legal foundation of our government’s fight against drugs of abuse. It provides a mechanism for substances to be controlled, added to a schedule, removed from a schedule or rescheduled. If a medication has a higher potential for all of the above factors it will require increased regulatory handling. This will affect the prescribing and dispensing of opioids, restricting as well as limiting the prescribing frequency and quantity of medication. The physician must review each patient’s risk to benefit ratio and document that in the patient’s chart.
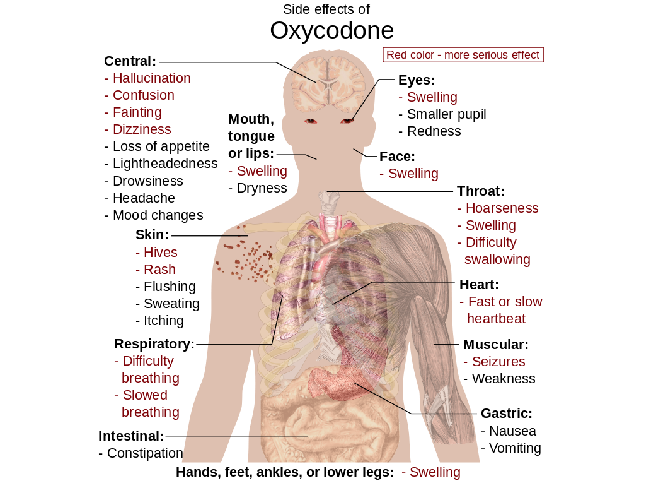
Common Side Effects for the Opioids can be seen in this chart listing those effects with the medication Oxycodone.
We started to see a movement during the 1990’s to be more aggressive in treating pain. There were supportive studies and reassurance from pharmaceutical companies that these medications were not addictive. Based on available data at the time less than 1% of the patients with chronic pain were physically dependent on an opioid medication. The medical community adopted this more aggressive model and began to use opioids to treat chronic non-cancer pain.
Fast forward to 2020. We have more people addicted to opioids than heroin and cocaine combined.
Addiction to a drug is defined as a compulsion to take the drug despite harm. Harm can be social, financial or psychological. The line between physical dependence and addiction sounds clear, but it is not.
In 2017 the number of opioid overdoses and deaths became alarming enough that the CDC labeled opioid overdosing as a national epidemic.
Additionally, there are complicated social and legal issues on opioids that point towards diminished benefits when administered over 90 days. Other concerns are family members stealing these medications from home for a non-medical use and patients selling their prescriptions. All of these issues as well as poly-pharmacy are a concern for drug misadventures and drug interactions – this puts more burdens on the prescribing physician to follow the guidelines for appropriate use of opioids. You can see why prescribing these medications have become more complex.
So let’s consider some advice for starting and/or continuing opioids;
- If you are on opioids and are concerned about addiction. You can talk to your provider to discuss and exit strategy to wean down opioids slowly over time or switch to safer alternatives. Be aware as with other common addictions this can involve short-term pain for long-term gain. The good news is that many patients who successfully weaned down their opioid use or stopped taking them have experienced improved function and mood as well as less pain overall.
- If you’re considering opioids for pain, make sure you have tried other safer alternatives first. If you decide to take opioids, try to limit use and set a date in the future to re-evaluate your symptoms. Take this time to discuss with your provider if therapy should continue, stopped or be changed. If your symptoms, such as pain and functionality, have substantially improved talk to you physician about stopping opioids. If you have seen little or no improvement in your symptoms, continue therapy and talk to your physician about alternative options.
- Reflect on your approach to pain. Take time every now and then to hit the reset button. It is important to look at non-medicinal forms of treatment such as activity, therapy, acupuncture, mind-body work and cognitive behavioral therapy to name a few options. Maybe add a new clinician to your team or see what a chronic pain clinic has to offer to replace your medications.
- To help your pharmacist provide you with the best care it is important to stick to one Pharmacy. Don’t increase your dose without talking to your prescribing physician. Have that information sent to your pharmacy so your communication with your insurance company will be streamlined when your next fill in being dispensed. Don’t combine opioids with other drugs such as alcohol.
- Make sure you keep your medication safe and out of reach from others. Keeping them in a locked box is a good idea.
Included is local information for safe medication drop off points to dispose of your unused medications;
To protect your privacy, please remove labels with personal information.
Clallam County
- Port Angeles Police Department
- Clallam County Sheriff’s Office
- Jim’s Pharmacy, Port Angeles
- Chinook Pharmacy, Forks
- Forks Police Department
Jefferson County
- Jefferson County Sheriff’s Office Port Hadlock. Mon/Tue/Thurs/Fri, 9m-4pm. Wed. 1-4 pm.
Grays Harbor
- Aberdeen Police Department has installed a prescription medication drop box in their lobby to dispose of unused medication.
Chronic pain is a condition that needs to be treated but it is important to be aware of the background on the concerns about taking opioids so you can make better decisions.
